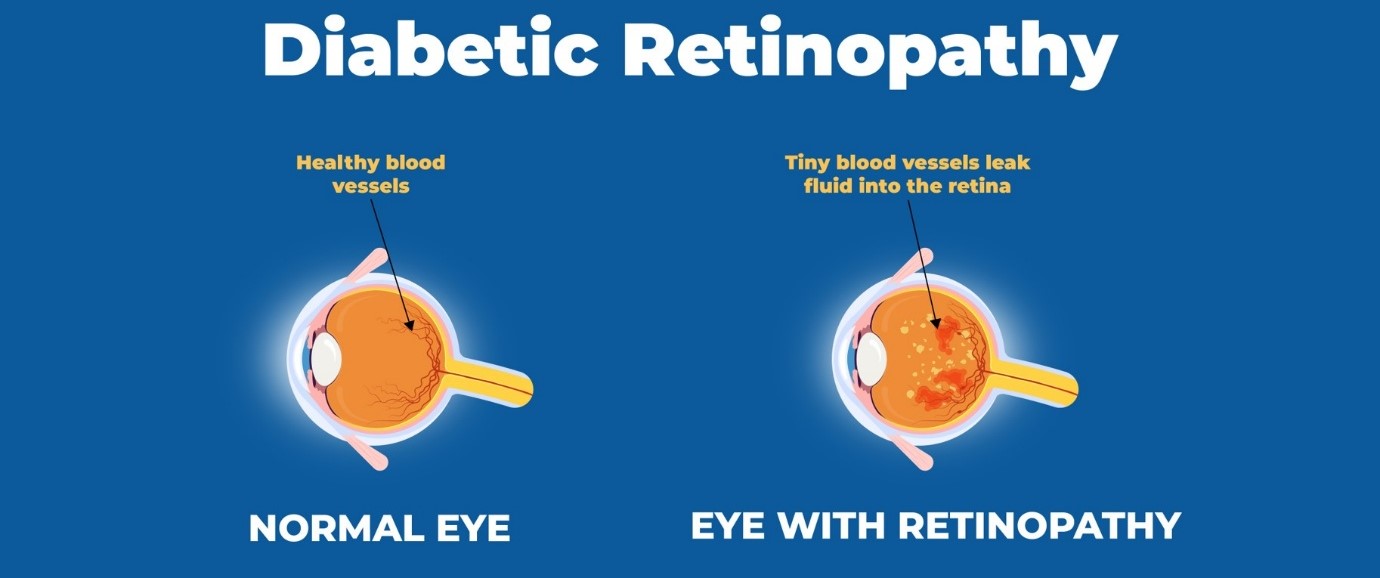
Diabetic Retinopathy is a serious diabetes-related eye condition that affects the retina, the light-sensitive tissue at the back of the eye. It occurs when high blood sugar levels damage the small blood vessels in the retina, leading to vision impairment and, in severe cases, blindness. This condition progresses gradually, often without noticeable symptoms in the early stages, making regular eye checkups crucial for early detection and management.
Symptoms of Diabetic Retinopathy
The signs of diabetic retinopathy often don't appear until significant damage has occurred inside the eye. Recognizing the symptoms early can help prevent severe vision loss.
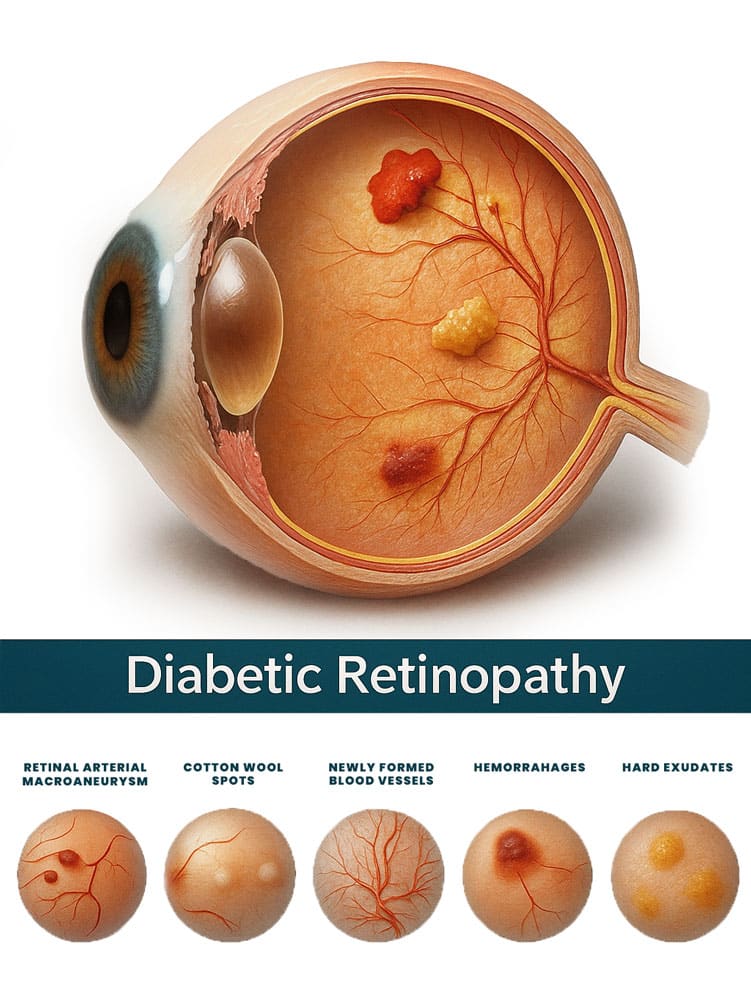
- Blurred Vision or Loss of Vision: As the diabetic retinopathy stages progress, the damaged blood vessels may leak fluid into the retina, causing blurred vision.
- Seeing Floaters or Dark Spots: Dark spots or floaters appear when bleeding occurs inside the eye due to diabetic retinopathy, blocking light from reaching the retina.
- Difficulty Seeing at Night: Patients may struggle with night vision due to decreased light sensitivity, which is one of the signs of diabetic retinopathy.
- Difficulty Distinguishing Colors: As retinal cells become damaged, it may become challenging to differentiate between colors.

Causes of Diabetic Retinopathy
The primary diabetic retinopathy causes include prolonged high blood sugar levels and associated conditions.
Stages of Diabetic Retinopathy
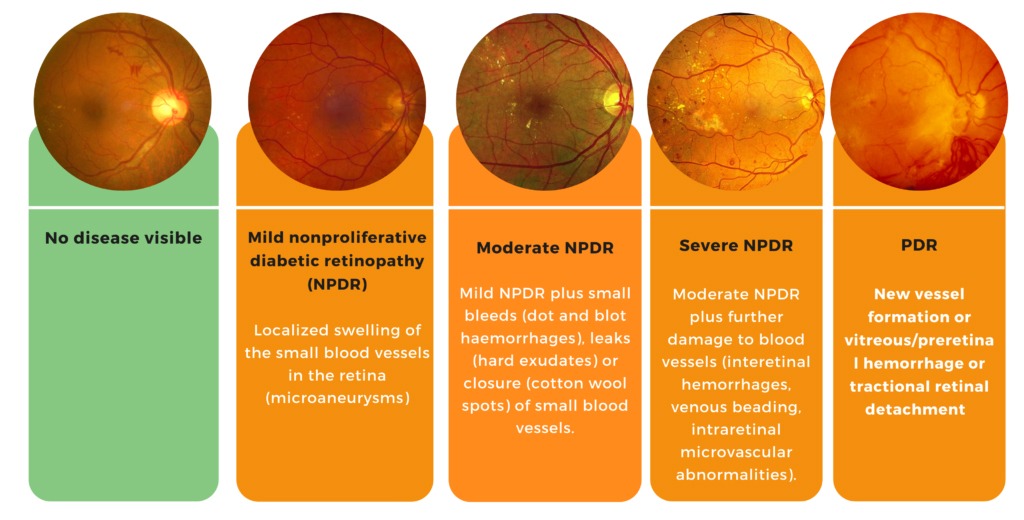
The damage occurs in four stages:
- Mild Nonproliferative Retinopathy: Small bulges form in the blood vessels, causing leakage.
- Moderate Nonproliferative Retinopathy: Blood vessels swell and distort, further restricting blood flow.
- Severe Nonproliferative Retinopathy: Blocked blood vessels deprive the retina of oxygen, leading to new, fragile vessel growth.
- Proliferative Diabetic Retinopathy: Advanced stage where new blood vessels form abnormally, leading to severe vision impairment.
Diabetic Retinopathy Risk Factors
Several factors increase the risk of developing diabetic retinopathy:
- Uncontrolled blood sugar levels
- High blood pressure and cholesterol
- Long-term diabetes (Type 1 or Type 2)
- Smoking and poor lifestyle habits
- Pregnancy-related diabetes (Gestational Diabetes)
How to Prevent Diabetic Retinopathy?
Preventing diabetic retinopathy involves maintaining overall eye health and managing diabetes effectively:
- Control blood sugar levels through a healthy diet and medication.
- Monitor blood pressure and cholesterol to reduce strain on blood vessels.
- Have regular eye exams to detect early changes in the retina.
- Quit smoking to improve circulation and eye health.
Management of Diabetic Retinopathy
Effective management of diabetic retinopathy depends on the severity of the condition:
- Mild cases require regular monitoring and blood sugar control.
- Moderate to severe cases may require laser therapy or injections to reduce swelling.
- Advanced cases often require vitrectomy surgery to remove blood and prevent retinal detachment.